On an ambulance boat in Jonglei state, South Sudan, Doctors Without Borders/Médecins Sans Frontières (MSF) teams rush four critically ill patients to the MSF hospital in Old Fangak. Among them is two-year-old Nya Thor, who is suffering from severe malaria—one of the leading causes of death in the country.
This is the second time that Nya Thor has become infected with the disease. According to her mother, Nya Sibet Mar, more and more people have become sick with malaria since heavy floods started in 2019.
“Two years ago, our house was completely flooded, so we had to look for another place,” says Nya Sibet Mar. “We arrived in Toch, but because there is more water than before, we live surrounded by mosquitoes. We see a lot of malaria cases now compared to before the floods.”
The young nation of South Sudan has seen the worst floods in the region over the past four years, exacerbated by change. During the rainy seasons, floodwaters have swept away entire villages, destroyed crops, drowned cattle, and severely damaged infrastructure, while forcing hundreds of thousands of people from their homes.

Children and pregnant women are especially vulnerable
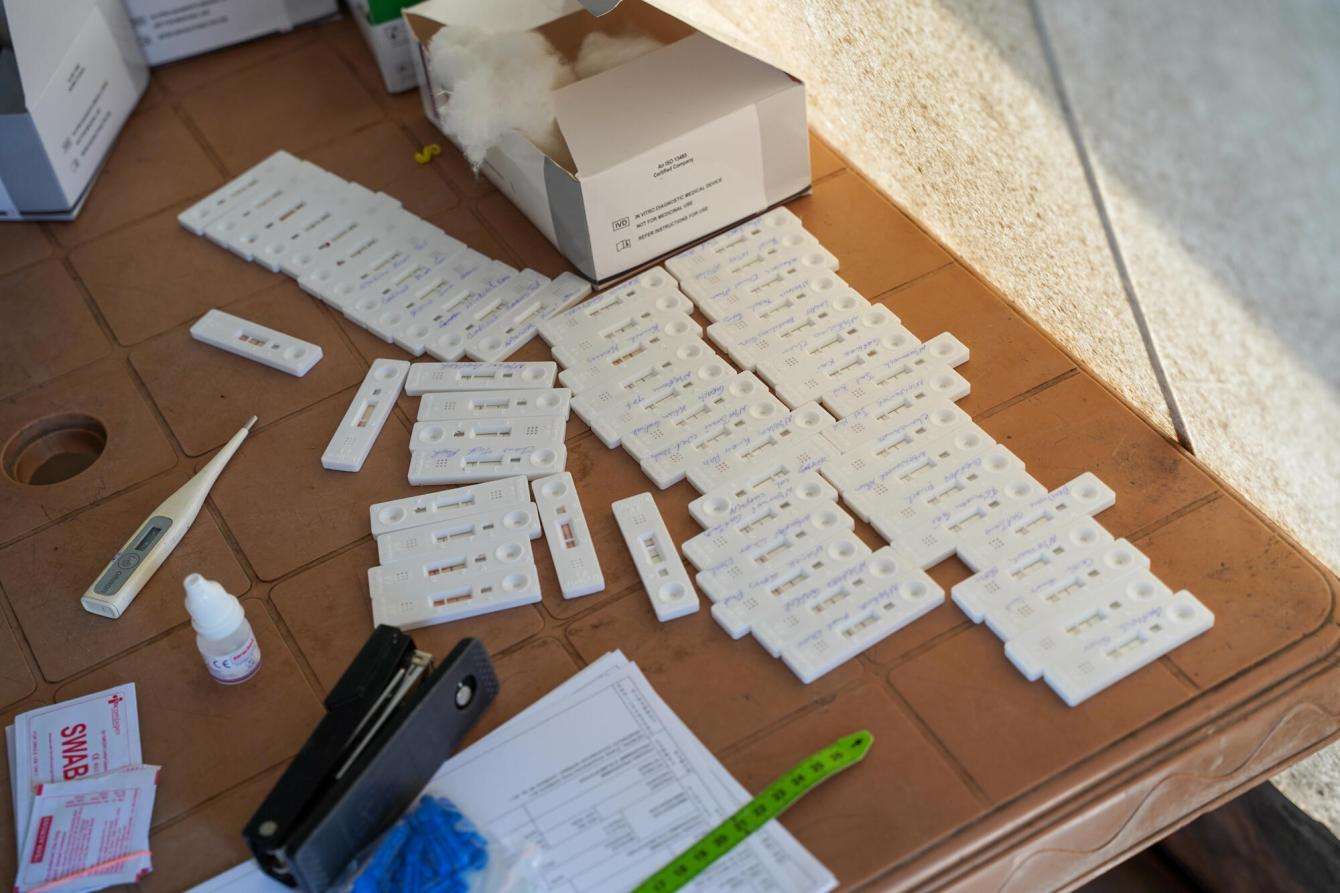
In Old Fangak, MSF teams are recording high numbers of malaria cases, especially among children and pregnant women. Since the beginning of August 2023, out of an average of 200 consultations per day, about 75 percent result in a positive malaria diagnosis. Each day, MSF teams admit 10 to 15 patients suffering from severe malaria.
In the hospital, MSF teams see both uncomplicated and severe malaria cases, and provide anti-malaria drugs, as well as treat complications such as severe vomiting, high fever, convulsions, pneumonia, anemia, and malnutrition. Nya Thor was admitted to the pediatric ward, where she receives treatment for malaria, malnutrition, and complications.

Floods bring rise in malnutrition cases
“Recurrent floods have aggravated malnutrition in Jonglei state, destroying crops and cattle and forcing communities to flee their homes,” explains Thomas Kun, a clinical officer who has been working with MSF since 2015.
“Families who used to cultivate crops now completely rely on fishing and food distributions from international aid,” says Kun. “However, due to the delayed rains, fishing is becoming more difficult, and international aid food distributions are not always consistent. Children, in particular, are suffering from not having access to food with adapted nutrients needed for their age.”
Communities cut off from health care
In addition to the lack of food, remote communities have been finding themselves cut off from health care and mosquito net distributions, putting their lives at additional risk. When people inevitably become sick, it takes several days by canoe to reach a medical facility for effective treatment. By then, uncomplicated cases may become severe, and pregnant women are among the most vulnerable.
“The infection can be directly transmitted from the mother to the fetus, but above all, high fever can terminate the pregnancy or induce premature labor,” explains Harriet Wikoru, MSF’s midwife activity manager at Old Fangak Hospital. “We give mosquito nets at prenatal care consultations. Many mothers, though, who live in very remote areas, are not protected.”
“As soon as we have a positive test for malaria, we immediately treat it,” adds Wikoru. “We cannot wait because we know the dangers of malaria for the mothers and their babies.”
After three days of medical care at the MSF hospital, Nya Thor and her mother are brought back to their village on MSF’s ambulance boat. That day, the MSF outreach team conducts malaria screenings, finding 42 positive cases out of 56 tests. Some patients are referred to the MSF hospital for treatment.
Malaria is a recurring disease that requires prevention measures
“Malaria is a disease for which you cannot immunize people. If mosquitoes get you again, then you will be reinfected,” explains Thomas Kun. “We keep treating patients, but nothing can ensure they will not come back after one month, infected again with malaria. We provide mosquito nets and blankets, but we have already seen patients coming back two, even three times these last few months.”
Old Fangak is not the only region in South Sudan badly affected by the recurring floods. Many areas in Unity and Upper Nile states, where MSF also has medical activities, have been restricted by floodwaters and turned into small islands surrounded by stagnant floodwater. Although this year, the rainy season and expected flooding in South Sudan seem to be delayed, our teams fear that malaria cases will continue to increase. The challenges of accessing and treating patients may worsen if expected floods isolate communities even further in Old Fangak and across the country.
To save lives from malaria, there is an urgent need to help communities better protect themselves by increasing distributions of mosquito nets and malaria medication, as well as access to health care and prevention measures in communities, especially for children and pregnant women. Because malnourished children are more vulnerable to severe malaria, children should be properly screened for malnutrition, enrolled in nutrition programs when appropriate, and receive their recommended vaccinations for childhood diseases.




