After Séverine gave birth to her seventh child, she knew something was wrong. She went to see a doctor at the Doctors Without Borders/Médecins Sans Frontières (MSF) health center in Gitega, Burundi.
“The MSF team welcomed me to the women’s village,” she says. “I feel good here; we dance together often. All the women here suffer from the same thing, and that helps us cope.”
“I’m having the surgery in a week. I hope it will go well; I’m confident it will.”
Two Million Women
Séverine is one of two million women worldwide with an obstetric fistula, a hole between the vagina and the bladder or rectum, through which urine or feces leaks continuously.
They are devastating injuries resulting from complicated childbirths. Often, the baby does not survive.
Trauma and Treatment
MSF surgeon Dr. Geert Morren explains the devastating impact a fistula can have: “For the mother, it’s a traumatizing experience. Not only does she go through a long and difficult birth, but she also loses the baby and ends up with a fistula that makes her incontinent.”
The injury can impact the rest of her life; women with fistulas are often excluded from social circles, sometimes rejected by friends and family.
Thankfully, most cases of fistula can be treated using surgical procedures. MSF teams treat hundreds of women every year, helping them return to their normal family lives.
Who Is Affected?
Poor women are the worst affected. Some estimate that 100 to150 women contract a fistula every day.
“Fistulas are most common in places where women don’t have access to health care,” says Dr. Morren, adding that a woman is unlikely to contract a fistula if a skilled attendant is present when she gives birth.
“Unfortunately, repairing fistulas is not a procedure that many local surgeons wish to do,” admits Dr. Morren. “First of all, it is technically quite difficult to carry out. Though it doesn’t require sophisticated equipment, it takes some time to master the technique.
“Secondly, it’s not well-remunerated because most of the patients are poor.”
As there will never be enough surgeons to help all fistula sufferers, preventing fistulas from occurring in the first place, by providing quality obstetric services, is key.
This presents MSF with a difficult choice: should we train gynecologists to treat fistulas, or should we focus on ensuring women have trained assistants present during childbirth?
In other words, should MSF prioritize prevention? How do we resolve this dilemma?
Preventing Fistula
“MSF won’t open a project that treats fistula without also investing in prevention,” says Dr. Morren.
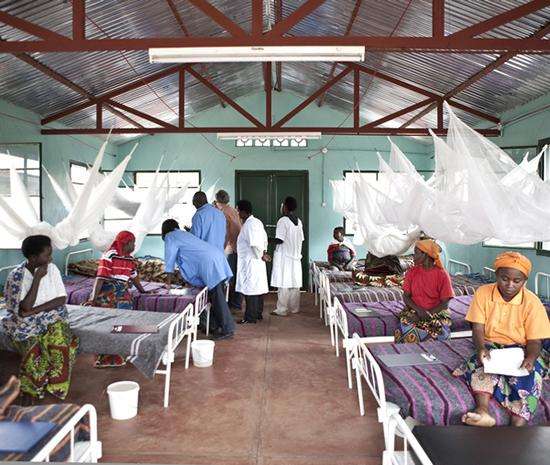
“For example, in Burundi, our teams opened a specialist obstetric clinic in Kabezi and a center for fistula treatment in Gitega. Since the beginning of the project, more than 1,000 patients have had surgery for fistula there.”
Returning Home
Séverine will soon be added to that number, and thus given a chance to live a normal family life.
“I’d like to go back to my family as soon as possible,” she says. “My husband supports me, as he feels just as responsible as I do for my pregnancy.
“That said, I do not hold it against my child. On the contrary, I am so happy that he survived. Many women die during a difficult labor.”
Success and Hope
We can help many more women like Séverine. According to Dr. Morren, MSF teams can play a lead role in training gynecologists to treat fistulas.
“We have invested a great deal in training Burundian surgeons in Gitega,” he says. “If we can train enough of them to allow us to hand over the caseload and leave, we’ll call this a success.”
MSF has three permanent centers in Chad, Burundi, and Nigeria to treat fistulas.